NKF Survey and Kidney PATH Program: Education is Key to Addressing Home Dialysis and Transplant Awareness Disparities Among Patients

Summary
In a recent survey of ESKD dialysis patients in partnership with NKF, education was found to help close disparity gaps in awareness of home dialysis or transplant as treatment options among various racial and ethnic groups. NKF Michigan’s successful Kidney PATH program is piloting an educational curriculum to help reduce these perceived barriers.
It is well established that access to education about available dialysis options is crucial to minority and socioeconomically disadvantaged communities with end-stage kidney disease (ESKD)—populations that are disproportionately burdened by health risk factors for chronic kidney disease, and kidney failure. For instance, black ESKD patients are less likely to receive any pre-ESKD nephrology care (63.2%) than white patients (69.6%), which is associated with a higher risk of initiating dialysis in the hospital, and lower likelihood of selecting home dialysis as a treatment modality, according to the United States Renal Data System. To gain a better understanding of the reasons for these disparities and explore workable solutions, the National Kidney Foundation (NKF) and Outset Medical partnered with Hanover Research to conduct an online survey of 450 black, white, and other ethnicity ESKD patients—NKF members or from affiliated sites—who had initiated dialysis within the past 10 years.
In key survey findings, there appeared to be no racial disparities in adoption of home dialysis among patients who were connected to kidney disease educational organizations. However, socioeconomic factors did contribute to differences in early knowledge of kidney disease status and opportunities for early education prior to kidney failure.
The overall theme of the NKF/Outset survey results is that almost all patients noted they are aware of both in-center and at-home dialysis options, as well as kidney transplant, which may be a result of surveying a relatively small, educated audience. The survey included patients 18 or older, with 38% of respondents being black, 52% white, and 10% another ethnicity, with transplant recipients excluded.
“What we can learn from the results from this small sample of educated ESKD patients is there were no underlying race or ethnicity factors that would cause somebody to choose in-center over home dialysis. Rather, it’s more a construct of lack of education, as well as some socioeconomic factors that are barriers,” says Tonya Saffer, Outset Medical’s Head of Government Affairs and Market Access, who worked with NKF on the survey design.
Respondents older than 50 and with incomes of $75k or greater were found to be more likely to ease into dialysis, indicating that they were more aware of their kidney disease, while those younger than 50 and with incomes less than $75k were more likely to experience an unplanned or emergency start to treatment. More patients overall, however, are currently receiving in-center hemodialysis (67%) than at-home dialysis (42%), though respondents with higher annual household incomes are more likely to currently receive at-home dialysis than those with lower incomes. (See Box for additional survey findings regarding at-home dialysis.) Thus, socioeconomic factors, as supported by published literature, also appear to play a role in the disparities in awareness and utilization of treatment options such as home dialysis or kidney transplant.
RACIAL DISPARITIES IN DIALYSIS PATH TO TREATMENT SURVEY: PATIENT USE AND PERCEPTIONS OF HOME DIALYSIS
Selected results:
- Among those aware of home dialysis: patients are about equally likely to currently receive either home hemodialysis (HHD; 20%) or peritoneal dialysis (PD; 25%), although participants have more previous experience with PD (18%) than HHD (7%)
- There are no notable racial group differences on care team encouragement towards trying either HHD or PD
- Among those aware of but not currently receiving home dialysis, 41% have discussed the option with their care team in the last 6 months, 26% have most recently discussed it 1-2 years ago, and 10% have never discussed it
- Patients who are aware of HHD cite the lack of required travel (51%), the ability to complete treatment in their own home (51%), and flexibility in choosing a day/time for dialysis (47%) as advantages
Source: Hanover Research, on behalf of Outset Medical and the National Kidney Foundation
Based on the survey results, NKF and Outset are also working together to ensure more patients get connected to education to better manage their kidney disease earlier and on their options for a kidney transplant and home dialysis to make a difference in reducing disparities. The organizations have developed a treatment-focused educational curriculum for kidney disease patients, that will be piloted in June as part of a core curriculum offered by the successful National Kidney Foundation of Michigan (NKFM) community health outreach program.
Survey Results Emphasize Impact of Socioeconomic Status and Education
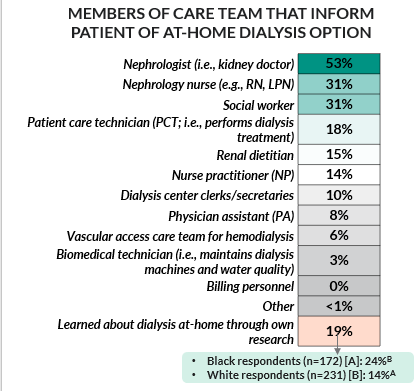
Importantly, results indicate that education provided outside the traditional healthcare setting, such as from external organizations like NKF, can play an important role in closing the racial gaps in home dialysis access and utilization. Patients of all backgrounds said that they refer to kidney disease-specific websites and/or health information websites before and after speaking to a medical professional, as well as patient information pamphlets. Overall, respondents indicated that their nephrologist provided education information on treatment options, along with renal dietitians, social workers, nephrology nurses, and other care team members (see the graphic below). Patients in all racial groups surveyed found the information provided by their care team to be useful, comprehensive, and proactively provided, although white respondents were more likely to do their own research following conversations with medical professionals.
Although a lower priority overall, white survey respondents were more likely than black respondents to place value on recommendations from physicians/nurses, suggesting that black respondents rely less on medical professionals. This is reinforced by findings surrounding trust in healthcare; white respondents were more likely than black respondents to fully trust healthcare providers more broadly, including when asked about their own providers. When selecting a dialysis treatment option, effectiveness and quality of life provided were most important to all patients in the study.
Kidney PATH Program to Include Pilot Educational Component Developed by Outset Medical
Outset Medical, as part of its ongoing commitment to working with the kidney care community to reduce disparities in treatment access for all ESKD patients and to increasing confidence in home dialysis, is taking additional steps to directly apply the knowledge gathered from this survey. Outset has provided a grant to NKFM to develop a curriculum that will be offered as part of the latter’s Stanford University-accredited, evidence-based chronic kidney disease self-management program, Kidney PATH (Personal Action Toward Health).
The purpose of the updated Kidney PATH curriculum will be to help empower people with kidney disease to better understand their options for home dialysis and transplant, and feel confident in selecting those as options for treatment. The core Kidney PATH curriculum, that is currently delivered to patients over six sessions, with one 2.5-hour session per week (in a virtual format for now), includes elements of the long-established Stanford PATH program. The new treatment modalities-specific content will be delivered via two additional curriculum pilot sessions, beginning this June.
“What’s exciting is that although this program is being piloted in Michigan, it really applies nationwide.”
-Tonya Saffer, Outset Head of Government Affairs & Market Access
NKFM has a long and successful track record of providing community-based health programs that bring together underserved populations, healthcare providers, and commercial payers. The organization has held educational sessions focused on diabetes and pain self-management, among other chronic health conditions, for many years. Stanford’s various PATH programs are delivered by many healthcare organizations across the country, with each session typically led by two trained leaders, at least one of whom has a long-term health condition. In the weekly sessions, participants learn strategies for better nutrition, healthcare options, and dealing with issues such as pain, fatigue, and difficult emotions. They also create personal action plans and set practical, achievable goals.
“NKF in Michigan has a lot of experience in addressing chronic health disparities, so they’re a really good partner for us in terms of implementing a kidney disease treatment education program,” says Saffer.
“Although the Kidney PATH program is excellent and very successful, what it was lacking was any education on what patients’ treatment options are when their kidneys fail, which is a key part of kidney disease self-management,” Saffer continues. She is working with other Outset team members and NKFM to develop and pilot the new curriculum. “If a patient is progressing into or is already in the advanced stages of kidney disease, it’s really important for them to understand that transplantation and home dialysis are options for them, in addition to in-center dialysis.”
“The goal with this new curriculum is to reach out to more disadvantaged populations, particularly those with lower socioeconomic status, and help them understand their treatment options, and how to overcome perceived barriers to home dialysis and transplant,” says Saffer.
As part of this educational initiative, Outset Medical will also assist NKFM in identifying and referring newly diagnosed CKD patients in Michigan to Kidney PATH courses where the new treatment-focused content will be piloted. Patients will also be surveyed pre- and post-program, with questions being added to evaluate the effectiveness of the new content in terms of changing knowledge, attitudes and willingness to do home dialysis.
“We will be evaluating post-course whether patients had a better understanding of their options, and whether they would be more or less likely to choose home dialysis, based on their participation in the curriculum,” says Saffer. She also notes that Outset will work with NKFM on publication of the results.
“What’s exciting is that although this program is being piloted in Michigan, it really applies nationwide. There is an opportunity for Outset to further collaborate with other NKF divisions to scale the program,” she adds.
In a related effort that points to the critical element of education in impacting the status quo in dialysis care, Saffer also recently co-authored a published NEJM Catalyst commentary, entitled “Bringing Kidney Care Home: Lessons from Covid-19.” The article notes that the pandemic made the expansion of home care essential for many diseases including kidney disease, and explores how to preserve and expand home dialysis. This includes suggested changes in regulations, education of both providers and patients, financial incentives to healthcare providers, and better coordination among the many federal programs devoted to improving kidney care.

